Original pediatric doctor Yan, pediatric doctor Yan
When I meet a baby with cough and wheezing, the first thing I think of is bronchiolitis (also called bronchiolitis), especially in winter and spring clinics.
Although bronchiolitis is not strictly pneumonia, it is difficult to manage, which is mainly related to its special lesion location and pathogenic pathogens.
01
bronchiolitis
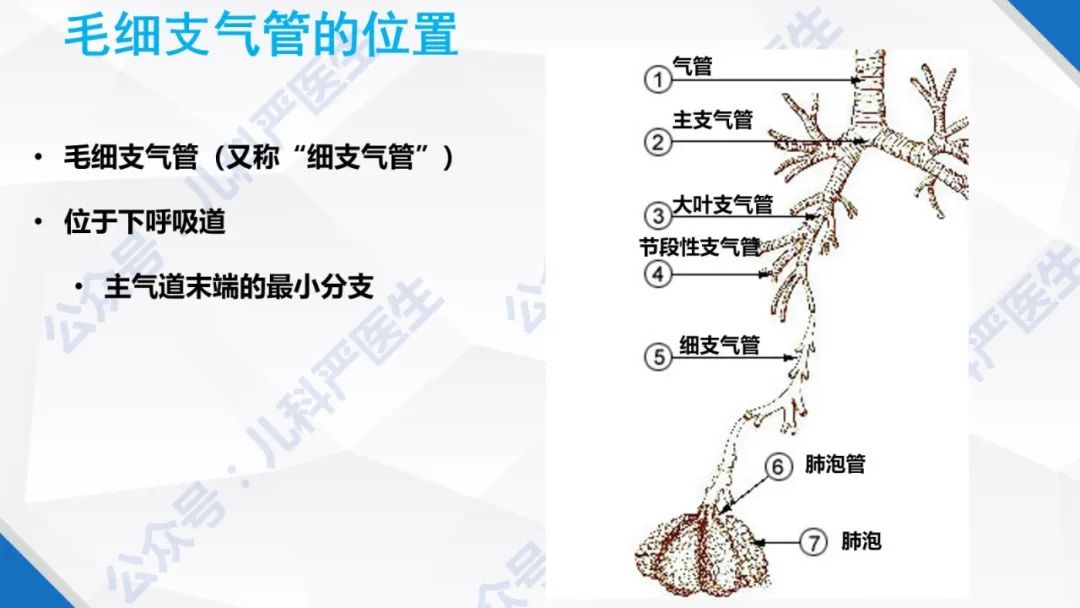
The bronchioles are located at the end of the bronchi (below ⑤, close to the alveolar ducts), and then down are the alveolar ducts and alveoli.
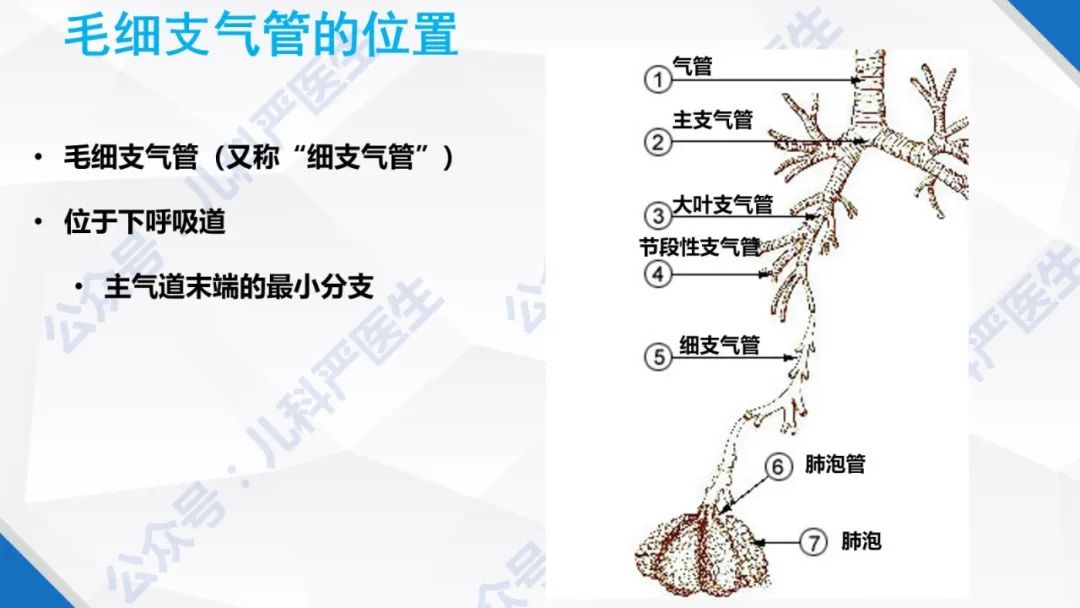
The respiratory tract of young children (especially infants under one year old) is relatively narrow, and local inflammation and exudation of bronchioles can easily cause lumen blockage, hinder air from entering and leaving alveoli, and even lead to hypoxia and dyspnea in severe cases.

The symptoms of children with bronchiolitis have their own characteristics, so that clinical diagnosis can be made through symptoms and signs.
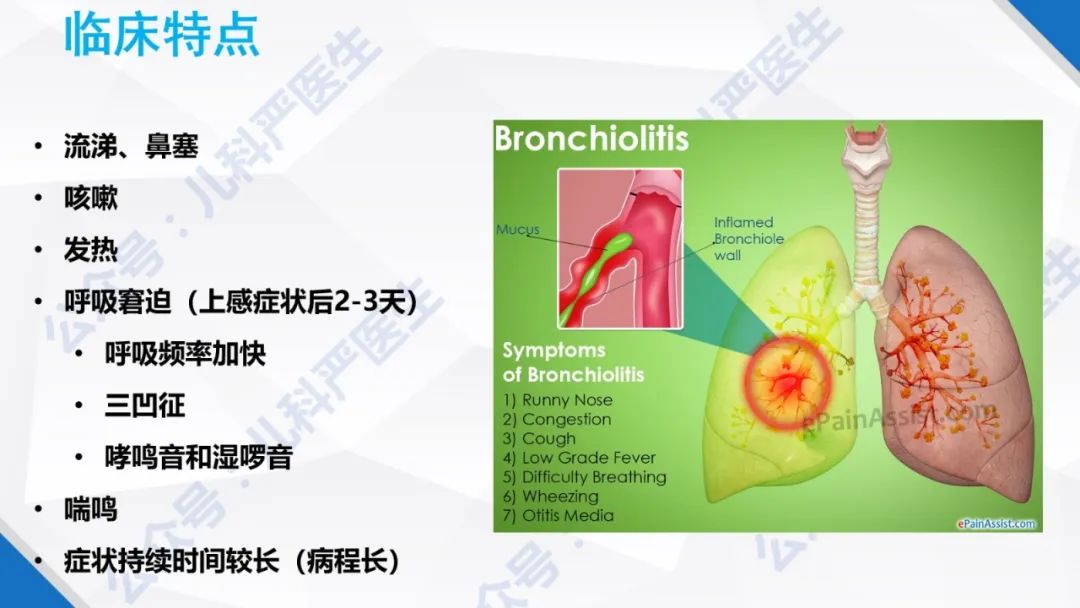
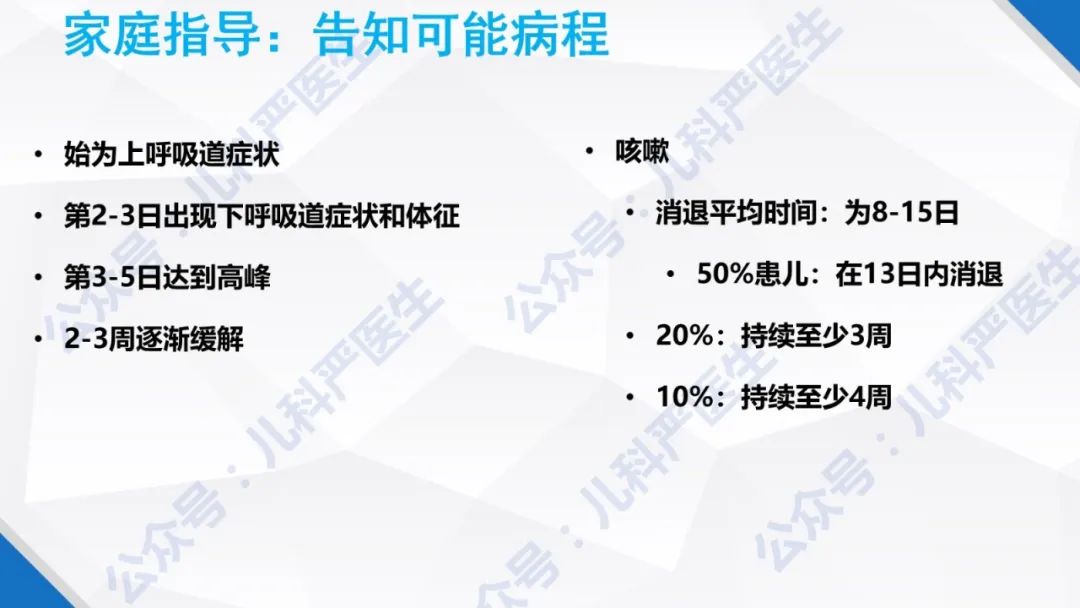
Early symptoms are mild, such as runny nose, stuffy nose, cough, and some have low fever, just like the common cold.
Different from the common cold, children with bronchiolitis have frequent cough and asthma in about 2-3 days, some have shortness of breath and inspiratory depression, and some have severe dyspnea.
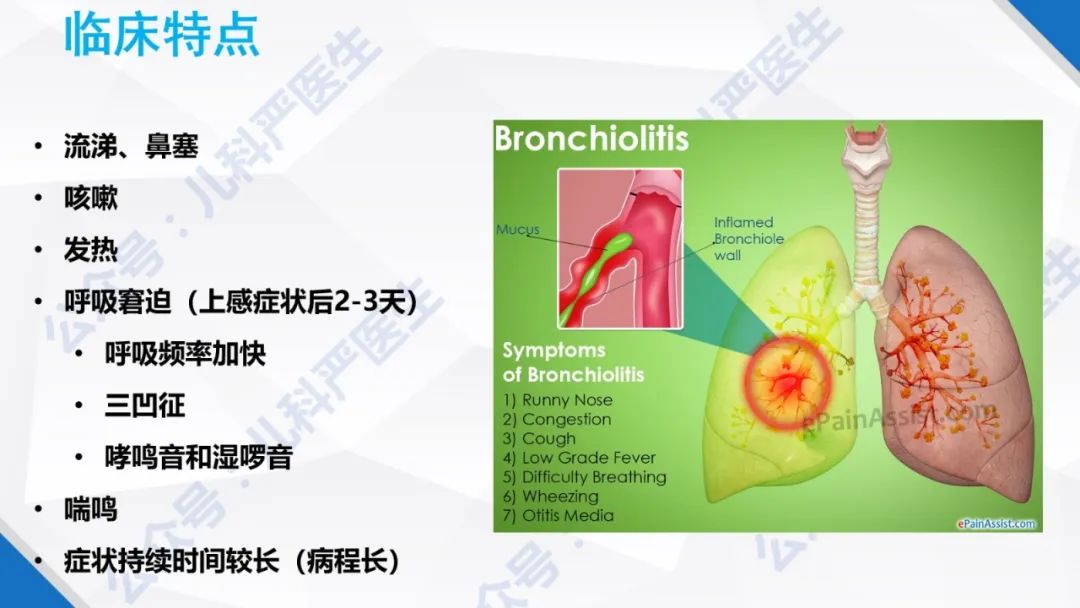
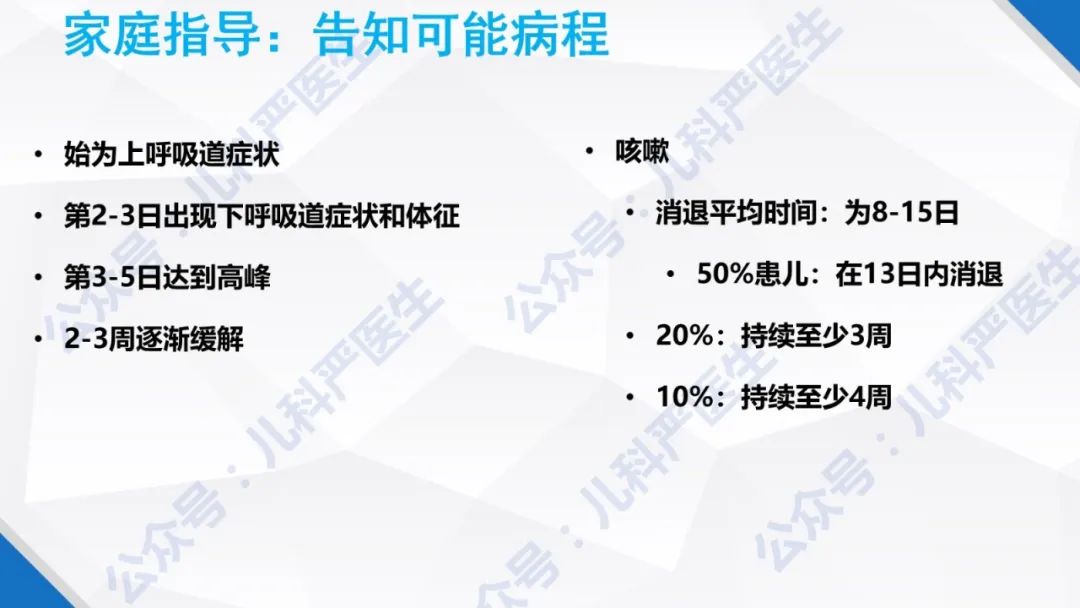
Then there is a long recovery period.
Although most children can recover by themselves (the course of disease is self-limited), some need hospitalization management and even use ventilator because of severe respiratory distress.

Bronchiolitis is mostly caused by virus infection, and there is usually no targeted antiviral drug, so it can only be treated symptomatically, and then the child can carry it by himself.
The main management measures include cleaning nasal secretions, ensuring liquid intake, high-flow oxygen inhalation and auxiliary ventilation when necessary.
Aerosol inhalation of bronchodilators (salbutamol, bricanyl) and corticosteroids (budesonide) has no obvious effect on bronchiolitis, and it is usually not routinely used continuously. Unless it is observed that the symptoms of cough and asthma in children are obviously relieved after atomization inhalation, they can continue, otherwise it is recommended to stop.
It is precisely because the drug treatment of bronchiolitis is limited, so the focus of management is not how to give drugs to children, but to guide parents.
For example, guide parents to care at home, observe the progress of the disease, identify severe cases, and let parents know that the next course of disease may be longer, so they must be psychologically prepared. Otherwise, children will face excessive intervention.
02
Significance of pathogen detection
Respiratory syncytial virus (RSV) is the most common pathogen causing bronchiolitis. In addition, rhinovirus, human metapneumovirus, parainfluenza virus, adenovirus and mycoplasma pneumoniae infection can all cause bronchiolitis.
If the child has typical bronchiolitis symptoms, it is unnecessary to check the pathogen. Because even if the pathogen is known, there is usually no antiviral method. But many times, I will choose to check.
Why check? Mainly to facilitate communication with parents.
For example, cough and asthma in children with bronchiolitis lasts for a long time, which may be several weeks, and has no obvious expected effect on many treatment methods including atomized inhalation. In this case, parents are inevitably anxious.
Parents are anxious and will try their best to control their children’s symptoms. They may take their children to see a doctor repeatedly, and the children will face more medication. In addition, repeated exposure to medical institutions will increase the risk of nosocomial infection.
And a clear result of pathogenic examination (such as detecting a virus) can alleviate parents’ anxiety to a certain extent and facilitate communication between doctors and patients.
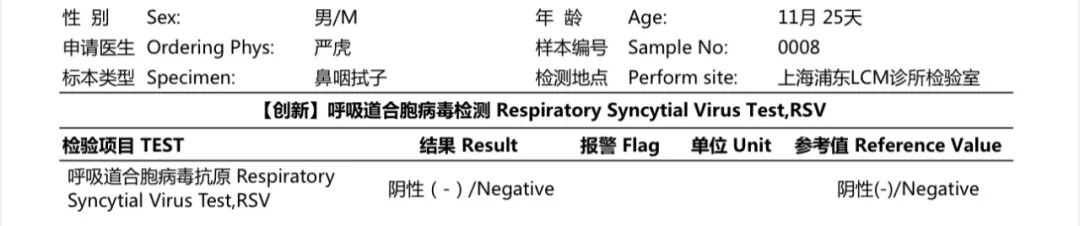
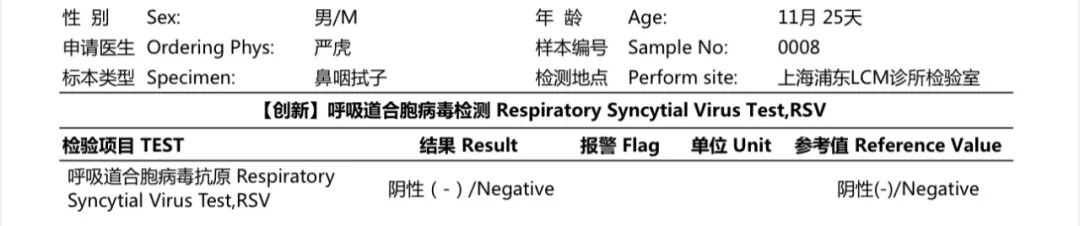
Therefore, in the clinic, when a child is suspected of bronchiolitis, I usually suggest a rapid antigen test for nasopharyngeal swab RSV first (RSV is chosen because it is the most likely and the rapid antigen test is very convenient).
If it is positive, inform the parents of the main points of home management, the possibility of facing a longer course of disease, and avoiding the abuse of antibiotics during this period, so that parents can be mentally prepared.
You see, proper auxiliary examination is actually to protect children.
However, RSV is only the most common virus that causes bronchiolitis. At work, children with typical bronchiolitis symptoms will also be encountered, but RSV is negative. How to manage it?
03
A case
Next, share a case. Before sharing, as usual, I would like to thank my parents for their permission.
This 11-month-old baby was the last patient on the afternoon of December 1st. Before coming to my clinic, the course of cough was nearly ten days, and I have been treated twice in other hospitals. In the clinic, the child coughed violently and vomited several times, with obvious asthma, shortness of breath and inspiratory depression, and fever.
Hormones and bronchodilators have been atomized and inhaled at home, and the symptoms are not obviously relieved.
I did a rapid RSV antigen test first, and the result was negative.
Although the child has shortness of breath and inspiratory depression, the degree is not serious and the oxygen saturation is still in the normal range.
Although coughing leads to vomiting and affects eating, there is no dehydration;
Although low fever, but the overall state is not bad, willing to interact with others, no symptoms of infection and poisoning;
Most importantly, my mother has a certain ability to observe the changes of diseases. Although she is anxious, she is not particularly anxious.
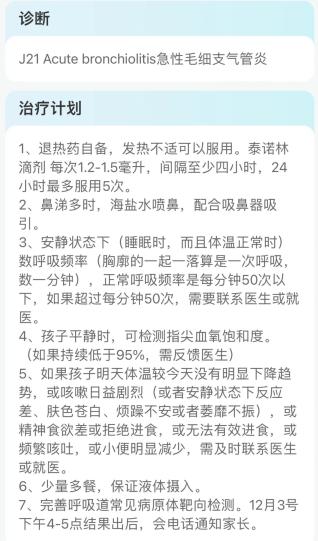
I evaluate that the child has not reached the indication of hospitalization at present, and there is no clear manifestation of bacterial infection. The high probability is still viral infection. After taking a throat swab sample and doing targeted sequencing, he didn’t prescribe medicine, so he was told to go home for observation and follow up online. I also repeatedly reminded that if the symptoms get worse, I need to be hospitalized.
To tell the truth, when the patient’s family was ready to leave the clinic after the visit, I was really sorry when my mother asked the children to wave goodbye to me. Coming from other places, the total cost of consultation and laboratory test is more than 1,500 yuan. I didn’t prescribe any medicine, and I didn’t know the pathogen. I went home empty-handed, and the future course of my illness is still unclear, which is really worrying.
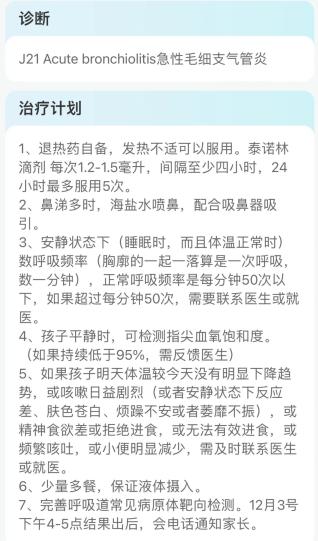
On the second day, I contacted my parents by phone. The parents reported that they still coughed and vomited, but the frequency was less, my temperature was normal, I could eat something, and my urine volume was normal.
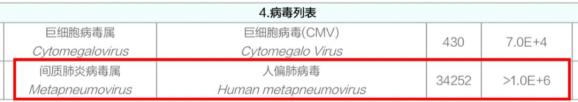
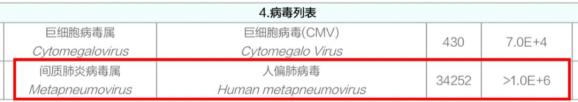
On the afternoon of the third day, targeted sequencing showed that the sample contained high concentration of human metapneumovirus, and cytomegalovirus was detected.
Combined with the symptoms of the child, I think the child is bronchiolitis caused by human metapneumovirus infection. As for the detected cytomegalovirus, it is considered to be carried in the pharynx (previous infection).
Because my home is out of town, I didn’t ask my parents to take her back to the clinic for follow-up, and I kept in touch by phone all the time.
Fortunately, the symptoms behind this child gradually eased, and it was not until mid-December that there was basically no cough, but there was phlegm in the throat from time to time. The total course of disease is more than 3 weeks, which accords with the characteristics of classic bronchiolitis.
04
Human metapneumovirus
Everyone should be unfamiliar with human metapneumovirus, and the doctor’s knowledge is likely to stay at the textbook level, because this pathogen is not checked at ordinary times and there is a lack of perceptual knowledge.
With the targeted sequencing in our outpatient department, many children were found to be infected with this virus. I thought it was a little strange at first, but if you look up the relevant information, you will find that you are rare and strange. I didn’t know it before, but I just didn’t have the ability to test it.

In 2001, Dutch virologist Bernadette G. van den Hoogen and his colleagues isolated a new virus from the respiratory secretions of 28 young children, named human metapneumovirus, hMPV).
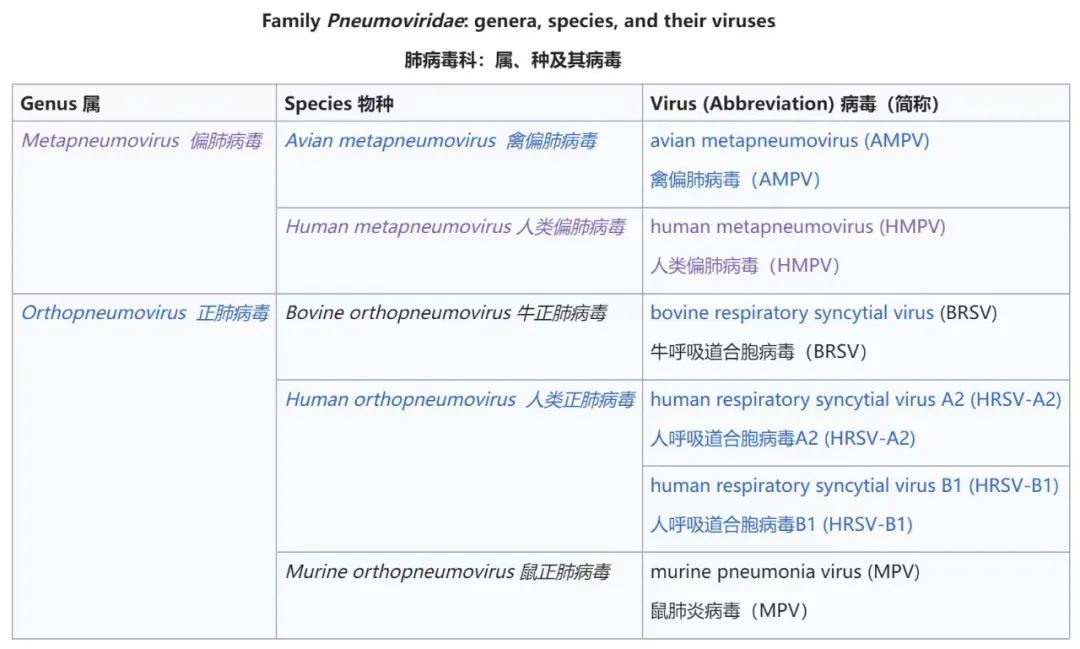
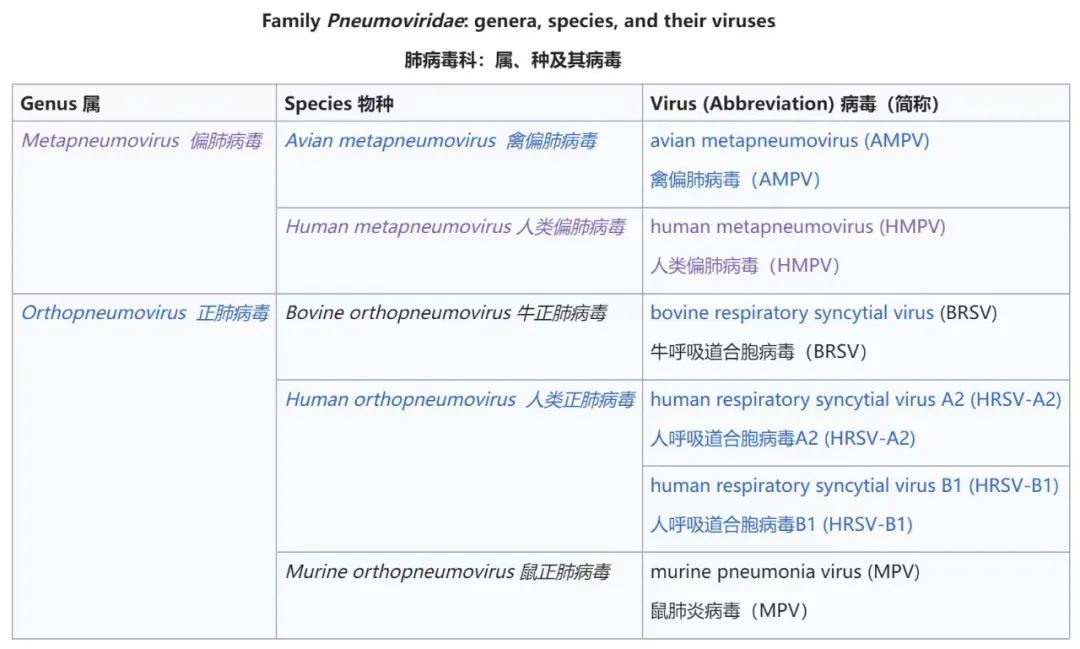
HMPV belongs to pneumoviridae. Pneumoviridae is named because its viruses are related to respiratory diseases of people or other animals, and the most famous one is RSV.
HMPV is distributed all over the world, and is often prevalent in winter/spring in temperate regions, overlapping with RSV and flu seasons.
Serological studies show that hMPV has spread for at least 60 years. By the age of five, almost all children in the world have been infected, which is considered to be the common cause of lower respiratory tract infection in children (second only to RSV in some areas).
Although infection is common in early life, reinfection is also common in older children and adults. Reinfection is mostly mild infection, such as common cold symptoms, but the risk of serious diseases will increase when reinfection occurs in immunocompromised people or the elderly.
HMPV may be transmitted by contact with virus-containing secretions, droplets, large aerosol particles or pollutants.
05
Symptom
The symptom characteristics and severity of hMPV are similar to RSV, so I often mistake hMPV infection in children for RSV infection.
Like RSV, the common symptoms of children infected with hMPV are fever, cough, runny nose and stuffy nose, and nearly half of young children may have asthma. A few patients may have acute laryngitis.
If hMPV only affects the upper respiratory tract, the symptoms are like common cold, such as mild fever, runny nose, stuffy nose, sore throat, cough and headache, which usually disappear in about a week.

However, hMPV is not very friendly to children and the elderly, and may spread to the lower respiratory tract. Infants infected with hMPV are prone to bronchiolitis, and the symptoms described in the first part of this paper, "Bronchiolitis", appear.
Some children with hMPV infection need hospitalization because of severe respiratory distress or inability to eat effectively with dehydration.
06
Severe risk
The risk of severe illness and hospitalization is significantly increased in the following groups:
Premature infants (gestational age ≤36 weeks)
Low birth weight infants (birth weight less than 2500g)
Infants under 1 year old
Chronic lung diseases (especially bronchopulmonary dysplasia)
Abnormal anatomical structure of airway
Congenital heart disease (with significant hemodynamic abnormalities)
Immune hypofunction
Nervous system diseases
Children with these high-risk factors need special attention, because their risk of adverse outcomes is significantly increased.
07
Treatment
Symptomatic treatment.
Use antipyretics to relieve discomfort caused by fever.
Clean nasal secretions to make children more comfortable and easy to eat and sleep.
Ensure liquid and energy intake and avoid dehydration.
Respiratory support: oxygen, assisted breathing.
Antiviral treatment.
Ribavirin and other antiviral drugs have been shown to be active against hMPV in vitro. However, there is no clinical data about the effect of ribavirin or other antiviral drugs on hMPV infection.
Therefore, antiviral drugs are not recommended for people infected with hMPV.
08
Epidemic vaccine
At present, there is no approved hMPV vaccine.
Moderna, an American pharmaceutical company, has developed a candidate vaccine against hMPV and conducted clinical trials.
As of October 2019, the candidate vaccine has passed the first phase of clinical trials. It is reported that the vaccine is well tolerated at all dosage levels within two months, and it stimulates immune response and produces neutralizing antibodies.
09
Total knot
Whether it is RSV, hMPV, or bronchiolitis caused by Boca virus, rhinovirus and parainfluenza virus, there is no difference in our management principles.
If you have the conditions to check, you can check the cause and find out hMPV, so don’t worry too much; If there is no condition to check, it can be diagnosed by symptoms and managed according to bronchiolitis.
The focus of management is still home care and observing the progress of the disease.
Original title: "Cough, asthma and fever, thought it was RSV infection, the result was human metapneumovirus, what should I do?" 》
Read the original text